With vaping on the rise globally, researchers are racing to understand how it affects the human body.
Marketed as a way to inhale nicotine with fewer of the harmful toxins present in cigarette smoke, electronic cigarettes are often perceived as less risky than traditional smoking and seen as a tool to help smokers quit. Are those claims scientifically sound?
The stakes are high. Nicotine is among the most addictive compounds on the planet. Vapes are being pushed by the same Big Tobacco industry that for decades hid the dangers of conventional smoking — which is now estimated to kill more than 7 million people each year worldwide. Consumers, healthcare professionals, regulators and voters are counting on accurate information on the true risks of e-cigarettes to make informed choices.
Some of the answers are simple and unambiguous. Experts agree that people who don’t smoke should not start vaping. They also agree that smokers would be better off quitting than switching from cigarettes to vapes.
But there’s little certainty on other important questions about e-cigarettes — including the long-term health impacts and how effective they might be at helping smokers quit conventional cigarettes.
Scientists don’t yet have many definitive conclusions, partly because e-cigarettes, or vapes, are relatively new, and the vast array of products are made of different ingredients and materials. Diseases that could be associated with their use could take decades to develop.
It’s no wonder you might be confused.
So how did The Examination approach these questions about vaping?
We set out to see what — exactly — scientific studies say about these questions.
I’m an experienced investigative journalist with a law degree — and still, at times, I found the quest for answers overwhelming, like navigating out of a desert with only part of a map. Search for “e-cigarettes” and other related terms on the website of the U.S.’s National Library of Medicine, and you’ll get over 11,500 hits for scientific articles.
Many studies are funded by government health and research agencies, or by nonprofit institutions. Some scientific journals publish tobacco industry-funded research when they consider it worthy, while others, such as the American Journal of Public Health, do not, having concluded that the tobacco industry’s longtime efforts to distort science show that the companies cannot be trusted. Science advances in small increments. It is not uncommon for academic articles to lead to different or contradictory conclusions — and seldom does a single study provide a silver-bullet, definitive answer.
After months spent interviewing experts and combing through studies and reviews (which are not the same thing), I reached a point where I can at least describe the map, even if gaps remain. (Reviews, by the way, are basically summaries of the research produced on a topic that often assess how conclusive the body of evidence is.)
Relying primarily on publicly funded work published since 2020, here’s what I found.
How do e-cigarettes work?
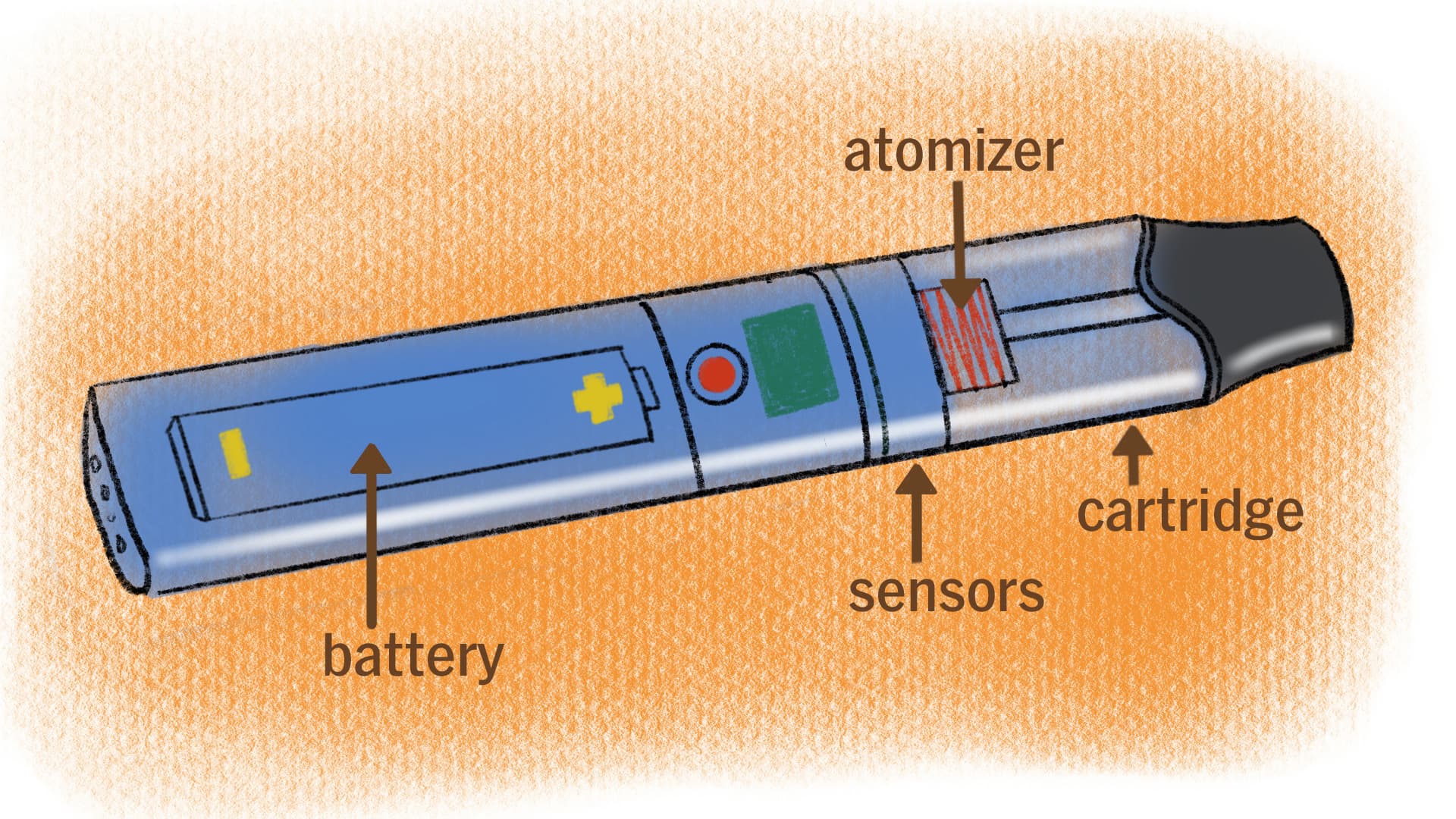
E-cigarettes or vapes are battery-operated devices that heat up liquids that usually contain nicotine, flavorings and other chemicals. As the e-liquids are heated, they are transformed into aerosols — or “vaporized,” thus “vaping” — that are then inhaled.
The amounts of the aerosol chemicals — some of them formed as the liquids get heated — may vary even for the same e-liquid, depending on the power and other characteristics of the device used. Metals present in e-cigarette parts can also transfer to the aerosols that users inhale.
E-cigarettes have evolved a lot since they first hit the marketplace in the mid-2000s, invented by Chinese pharmacist Hon Lik. Hon said in patent applications that the device would serve as a substitute for quitting smoking.
Current vapes are often much more effective at delivering nicotine than their predecessors, which could help some smokers trying to switch to e-cigarettes but also put nonsmokers — both teenagers and adults — at a higher risk of becoming addicted to nicotine.
For example, using nicotine salts — created by adding acids to a form of nicotine called freebase — allows manufacturers to increase nicotine concentrations because it makes inhaling the nicotine less harsh on the throat.
But other innovations may also affect nicotine delivery. Researchers found that JUUL-brand pods sold in Europe — where regulations limit nicotine concentrations in e-liquids — had a different design from U.S. pods. The modified versions delivered more vapor, and an amount of nicotine per puff close to the U.S. products, even if the nicotine concentration in the e-liquid was much lower.
Disposable e-cigarettes typically cost $5 to $20 in the U.S. and last for 600 to more than 7,000 puffs. Reusable vapes can range from $10 to more than $100.
What chemicals do vape users breathe in?
Short answer: Do you want to know the whole list? Scientists do, too.
There are thousands of e-liquids on the market, with a variety of chemical compositions.
The main components of vaping liquids are solvents such as propylene glycol or glycerol. Both are airway irritants and are considered generally safe by the U.S. Food and Drug Administration for eating — but have not been deemed safe for inhalation.

Many e-liquids also contain nicotine and flavorings. A single e-liquid refill may have dozens of flavor additives, and studies have identified thousands of e-liquid flavors on the market.
While many flavorings are generally considered safe for ingestion, like with the base solvents, there is no evidence that they are safe to inhale. One of the concerning additives that has been detected in some liquids is diacetyl, a flavor enhancer that has been linked to lung damage when inhaled.
Researchers have also identified particles of metals such as chromium, lead or nickel, that often come from the device, as well as contaminants such as arsenic in e-cigarette aerosols.
Then there are the chemicals formed as the e-liquids get heated up. One of those is formaldehyde, which, at certain levels, can impact the lungs, and is also classified as a human carcinogen by the International Agency for Research on Cancer. The compound is created when glycerol and flavoring components are heated.
Other troubling chemicals in the aerosols include carcinogenic tobacco-specific nitrosamines and ultrafine particles that penetrate deep into the lung, as well as other volatile organic compounds like benzene, also a carcinogen.
There’s little data on the harms that the potentially toxic chemicals could cause at the dosages found in vaping aerosols.
The toxicological profile of most e-liquid ingredients and aerosol components has not been fully investigated, according to a 2021 report by a European Union scientific committee.
Researchers from Johns Hopkins University analyzed the aerosols of four e-cigarette brands and found hundreds of chemicals they could not identify.
How do the chemicals in vapes affect your body?
Short answer: Scientists don’t know much, but have raised red flags.
Experiments in recent years have shown that e-liquid aerosols are toxic for cells cultivated in laboratories and harm DNA. Other studies suggest that they harm the respiratory and cardiovascular systems in mice. But those results don’t necessarily mean that humans will suffer the same effects.
Researchers did detect short-term cardiovascular effects in humans after the use of nicotine e-cigarettes, such as increased heart rates and arterial stiffness. But they couldn’t conclude whether vaping will cause long-term cardiovascular disease.
Urine and saliva from people who vape contained certain carcinogens at higher levels than samples from people who don’t vape or smoke, multiple studies found. Scientists say more research is needed in this field. It’s unknown whether vaping will cause cancer.
Experts are studying whether vaping may worsen asthma or damage the lungs in other ways.
Nicotine, often present in e-liquids, is a highly addictive chemical. One review said there is growing evidence showing that it can affect brain development in adolescents and is linked to poor impulse control and impaired learning. As of March, 2021, more than 250 reports of e-cigarette-associated seizures have been submitted to the FDA, a majority occurring in youth or young adults. Scientists disagree, however, on whether there’s enough evidence to show that nicotine vaping can lead to seizures.

E-cigarettes likely cause less serious health effects as well, according to a review by researchers at the Australian National University. The reviewers considered that there’s moderate evidence that nicotine e-cigarettes can cause headaches, coughing, throat irritation, dizziness and nausea.
Many diseases that could be associated with vaping may take many years to develop.
So … are vapes less harmful than regular cigarettes?
There’s no consensus, but much of the research I could find suggests that the answer is likely yes. That’s not a particularly high bar — the U.S. Centers for Disease Control and Prevention calls smoking “the leading cause of preventable death.”
But the question is somewhat flawed. It’s hard to assess precisely how e-cigarettes compare because their ingredients and types vary so widely — and it’s unclear how they will impact the body over time. Because of that, some researchers say it’s too soon to know if e-cigarettes are safer than cigarettes.
Studies do show that vaping exposes users to fewer of the toxic chemicals present in cigarette smoke, and generally at substantially lower levels.
An exception may be exposure to some metals. Urine and blood tests from people who vape showed similar levels of beryllium, uranium and zinc as those from smokers, several studies have found.
Health benefits that smokers may get from switching to e-cigarettes don’t seem to apply to smokers who also vape — a substantial proportion of those who use e-cigarettes. Some studies suggest that risks for dual users can be higher than for exclusive smokers.
A 2015 report on the safety of vaping commissioned by Public Health England stirred widespread controversy. It maintained that e-cigarettes are around 95% less harmful than conventional cigarettes. The percentage had appeared in a previous academic article and the report’s authors said it seemed reasonable. The estimate has since been frequently repeated by e-cigarette manufacturers and pro-vape groups and used to lobby for less restrictive regulations for e-cigarettes.
But that estimate has been criticized by public health researchers — and by an editorial in The Lancet, one of the world’s most prestigious medical journals.
Many health experts are also concerned that, after years of declining smoking rates, e-cigarettes could end up hooking many youths on nicotine.
The Lancet editorial pointed out conflicts of interest surrounding the original study’s funding and criticized its conclusion.
“The opinions of a small group of individuals with no prespecified expertise in tobacco control were based on an almost total absence of evidence of harm,” the editorial said.
The authors of the original report defended the expertise of the panel they convened to assess the dangers of the products and said funders of the study didn’t influence their assessment.
Last year, three authors of the 2015 report acknowledged that the 95% safer estimate could be simplistic and misinterpreted, and added some nuance.
“It might now be more appropriate and unifying to summarise our findings using our other firm statement: that vaping poses only a small fraction of the risks of smoking,” they said in an updated report co-authored by five other researchers.
Can e-cigarettes help smokers quit?
They are not approved by the U.S. Food and Drug Administration as smoking cessation tools. Yet, with clinical supervision, some nicotine e-cigarettes have been shown to help some people.
A 2022 review of six randomized trials by the Cochrane Collaboration — a nonprofit network of scientists recognized for its high standards — showed that people are more likely to stop smoking for at least six months by using nicotine e-cigarettes rather than using nicotine replacement therapy, which include products such as nicotine gums or patches. The review concluded there’s high certainty that e-cigarettes are more effective for quitting.
But other researchers say that evidence is not solid.
A 2023 review funded by public agencies in Australia concluded there’s limited evidence that with clinical support, freebase nicotine e-cigarettes are more effective than nicotine replacement therapies. The reviewers concluded there’s zero evidence about the efficacy of e-cigarettes that contain nicotine salts. Nicotine salts are typically present in some popular brand-name products, like JUUL.
The Australian reviewers used more stringent criteria, excluding results that hadn’t been published in a peer-reviewed article. They disagreed with the Cochrane review assessment and concluded that the trials were generally at a higher risk of leading to biased or misleading results.

A Cochrane review of randomized trials published last week estimated that for every 100 smokers, 10 to 19 are likely to quit using a nicotine e‐cigarette, compared to 6 in 100 of those who don’t use e-cigarettes or medicine.
The results also show that effectiveness of e-cigarettes is likely similar to the drug varenicline.
Studies also indicated that those using e-cigarettes to quit smoking were likely to keep vaping after quitting smoking. Globally, 70% of those given an e-cigarette to help them stop smoking were still vaping at 6 months, according to one review that analyzed 19 studies.
Even in the U.K. and New Zealand, where health authorities have promoted vaping as a way to quit smoking, no e-cigarette products have been approved as medicines or undergone the scrutiny typically required to be sold as such.
Another debated question is how the results fare when the products are used in the real world without clinical supervision.
A 2021 review of observational studies concluded that people who used e-cigarettes, overall, weren’t more prone to quit smoking.
Does vaping make you more likely to take up smoking?
There’s no consensus about this one either.
Studies that survey people about whether they smoke or vape over time consistently show that young people who don't smoke but use e-cigarettes are more likely to take up smoking cigarettes later on than those who never vaped.
In these studies, researchers try to control for respondents’ traits or circumstances that could make them more prone to both vaping and smoking, such as gender, income, having impulsive behavior or living with a smoker.
Experts acknowledge that it’s hard to account for all those risk factors and that some studies account for them better than others, so results could still be influenced by them.
Subscribe to our newsletter
Global health reporting, straight to your inbox
Still, many conclude that the consistency of findings across studies supports the likelihood that vaping increases the odds for someone to take up smoking.
Sounds like we almost have an answer, right? Not so fast. It turns out not everyone reads the results the same way. Critics note that the studies’ shortcomings weaken the ability to determine causation.
What are countries doing about vaping?
Policies worldwide range from total bans on e-cigarette sales to a total absence of regulations. Some countries regulate e-cigarettes as tobacco products, restricting ingredients, promotion and indoor use. Australia allows the sale of nicotine vaping products to smokers with a doctor’s prescription — even though health authorities haven’t approved them as medicines.
In the United States, nicotine vaping products require authorization by the FDA.
The FDA has so far authorized 23 e-cigarette products — including devices and cartridges prefilled with e-liquid. But, according to a report from the tobacco control group Truth Initiative, as of September 2022, there were nearly 2,000 different products on the market. Most are sold illegally.
So, what does all this mean for you, your loved ones and your community? What should you be watching out for when you read about vaping?
We often think of science as an objective, almost mathematical process. We expect to get from it certainties, percentages, a clear yes or no. Yet science can be uncertain. Experts can interpret studies in different ways and disagree on the extent to which some support a specific point — or how strong or weak they are.
With e-cigarettes, there are many disagreements, but also a common goal: trying to figure out whether they can help reduce or eliminate smoking and if so, under what circumstances they could benefit the public.
Support The Examination
Help sustain independent journalism for a healthier world.
While some nicotine e-cigarettes may help some smokers quit, it doesn’t look like the devices and e-liquids tested in trials will be a saving grace for most smokers, even when used under clinical supervision. Any differences in how much more useful they could be compared to nicotine replacement therapies appear so far more incremental than revolutionary. On the other hand, if even a small percentage of smokers could benefit, that could still be a large number of people worldwide.
Many health experts are also concerned that, after years of declining smoking rates, e-cigarettes could end up hooking many youths on nicotine. In countries across the world, vaping rates are higher among teenagers than adults.
With the long-term health effects of e-cigarettes still poorly understood, regulators, lawmakers, smokers, consumers and parents face hard choices.
Researchers will keep working on getting the answers. And I will keep trying to make sense of it.

